
New Year’s Nutrition Resolutions from a Long Island Dietitian
New Year’s Nutrition Resolutions from a Long Island Dietitian
Dietary Interventions and Eating Behaviors for Sustainable Change
Though a New Year’s resolution signifies a new start, many people fixate on unrealistic goals that are…

Healthy Holiday Eating Tips from a New York Dietitian: Manage Your Health and Waistline
You can celebrate the holidays without leaving healthy eating behind. Enjoy the food and festivities. Most foods, even special holidays “treats”, can be part of a healthy eating plan. The key is moderation and mindfulness.
Long Island…
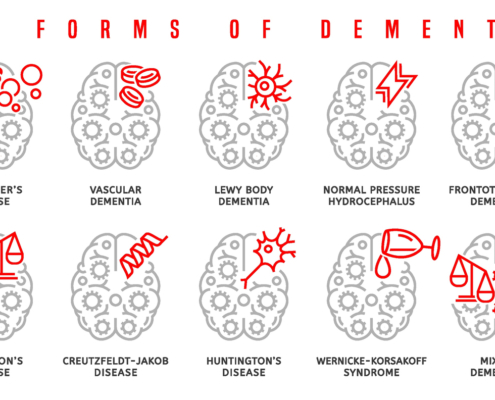
DEMENTIA PREVENTION SHOULD START AT MIDLIFE. The time to start is in your 40’s.
The link between brain health and nutrition is irrefutable. As a Long Island dietitian, I have spent my career working to help patients improve their wellness through individualized dietary interventions, and this includes providing evidence-based…
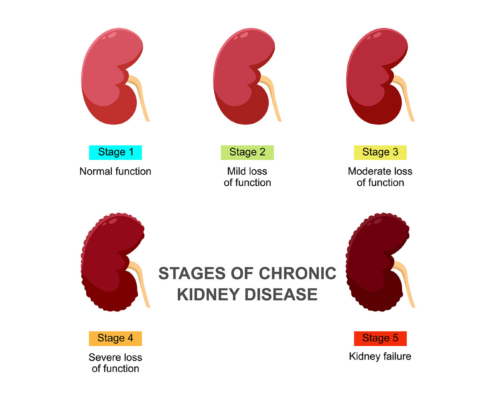
Can a Nutritionist Help with Kidney Disease?
What do diabetes and kidney disease have in common? Diet – they are both improved with the identical nutrition plan.
How do you keep your kidneys healthy when you have diabetes?
If you manage your blood sugar you reduce the likelihood…

What is Food as Medicine?
Food as Medicine is based upon the recognition that food and diet play important roles in disease prevention and management. The fact that diet can impact an individual’s health is now well documented and accepted by healthcare providers…

Holistic Nutritionist New York: What is a holistic nutritionist? Do you need one?
There is a growing number of people searching for holistic nutritionists, and there are many holistic nutrition practices. What is important to understand is that “holistic nutritionist” is not a credentialed title. Anyone can call themselves…

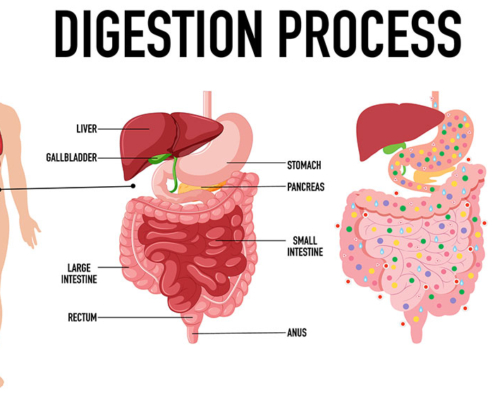
How to Improve Digestive Health
As I discussed and explained in previous blogs, there is a microscopic world that lives in your large intestine called the gut microbiome. It is made up of trillions of microorganisms. Though most are bacteria, there also are fungi and…
What is the Importance of Digestive Health? A Long Island Certified Dietitian Nutritionist Discusses Gut Health
Everybody is talking about “gut health”. There are whole sections of bookstores now dedicated to books on digestive health; aisles of grocery stores and products pushing digestive health antidotes, remedies, fixes, and more. Once you understand…

IS THE GLYCEMIC INDEX IMPORTANT IN 2024? Or is it Outdated?
To understand my answer, I need to explain the glycemic index, fiber, and processing:
What is the glycemic index?
By definition, the glycemic index is a measure of the blood glucose raising potential of the carbohydrate content of a food…
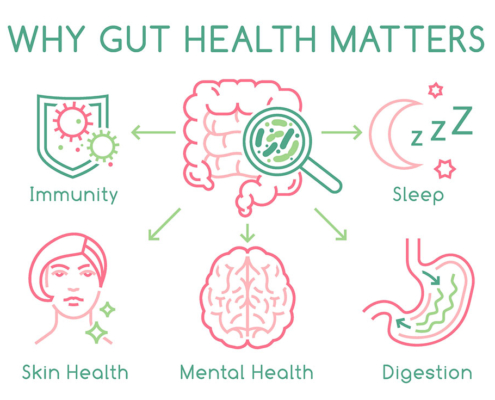
LEARN WHAT TO EAT TO HAVE A HEALTHY MICROBIOME
Why Gut Health Matters
As a registered dietitian nutritionist, I have worked with innumerable individuals over the years who struggle with digestive/gastrointestinal problems (gut health) such as Irritable Bowel Syndrome, Inflammatory Bowel…

Can a Dietitian Help You Lose Weight? What should you expect? Should you see a dietitian or a nutritionist?
In the New Year, it’s not uncommon to want to get healthier and lose those extra pounds. In fact, weight loss is a top resolution.
How do you lose weight?
Weight loss can be made very complicated, but this is unnecessary and counterproductive.…

What is the difference between a dietitian and a nutritionist?
With so many nutrition professions, it can be difficult to understand how they differ. This is especially the case for nutritionists and dietitians. The terms dietitian and nutritionist may sound similar, but there are significant distinctions: …
